Publications
Stopping Pain: Percutaneous (Per·cu·ta·ne·ous) Hydrotomy: A Revolutionary Approach to Beating Chronic Pain and Increasing Function
“Stopping Pain” introduces the groundbreaking world of percutaneous hydrotomy, a revolutionary medical technique developed over 30 years ago in France. This regenerative approach employs physiologic saline, vitamins, minerals, and carefully selected medications to alleviate chronic pain and enhance overall function.
In this book, you will learn:
- Understand the principles and mechanisms that make percutaneous hydrotomy an effective solution for chronic pain.
- Explore compelling narratives of individuals who, despite years of medication, found relief and regained their zest for life through percutaneous hydrotomy.
- Discover how both amateur and professional athletes, including NFL players, MMA athletes, motocross racers, cyclists, and professional tennis players, have benefited from percutaneous hydrotomy to overcome pain and enhance performance.
- Gain insights into how percutaneous hydrotomy offers a new ray of hope for patients grappling with chronic diseases, providing them with the potential for a pain-free and fulfilling life.
“Stopping Pain” is your guide to breaking free from the shackles of chronic pain and embracing a future filled with vitality and well-being. Don’t let pain dictate your life any longer—discover the transformative power of percutaneous hydrotomy.
The authors Johnathan Edwards MD and Bernard Guez MD
Vaincre les maladies chroniques par l'hydrotomie percutanée
Still little known, but existing for around twenty years, this technique offers an effective perspective to people suffering from chronic illnesses (including osteoarthritis, lower back pain, migraine, allergies, autoimmune diseases, etc.) or suffering from pain. relapsers, looking for a solution to relieve their pain.
Written by the founder of the technique, this new book aims to introduce percutaneous hydrotomy to the general public.
At the end of the book, a testimonial section is devoted to patients who have chosen this practice.
This book only exists in French.
The author – Bernard Guez MD
Established in Nice for around twenty years, he is a general practitioner. Specialized in mesotherapy, homeopathy, geriatrics, he is also a beautician and expert with from the HAS (High Authority of Health) in mesotherapy aesthetic. He has been practicing for almost 40 years and has carried out more than 350,000 sessions in general medicine interventional for all pathologies. Founder of the percutaneous hydrotomy technique, he regularly trains health professionals (doctors and nurses) from all over the world. He is also a member of the SIHP (International Society Percutaneous Hydrotomy) and occurs every year in the international annual congress
Presentation by Johnathan Edwards, MD of percutaneous hydrotomy at the 50th Annual ASRA Pain conference in Orlando, Florida
Presentation by Bernard Guez, MD of percutaneous hydrotomy at the 15th INTERNATIONAL CONGRESS OF MESOTHERAPY Tunis, Tunisia
Definition of Percutaneous Hydrotomy
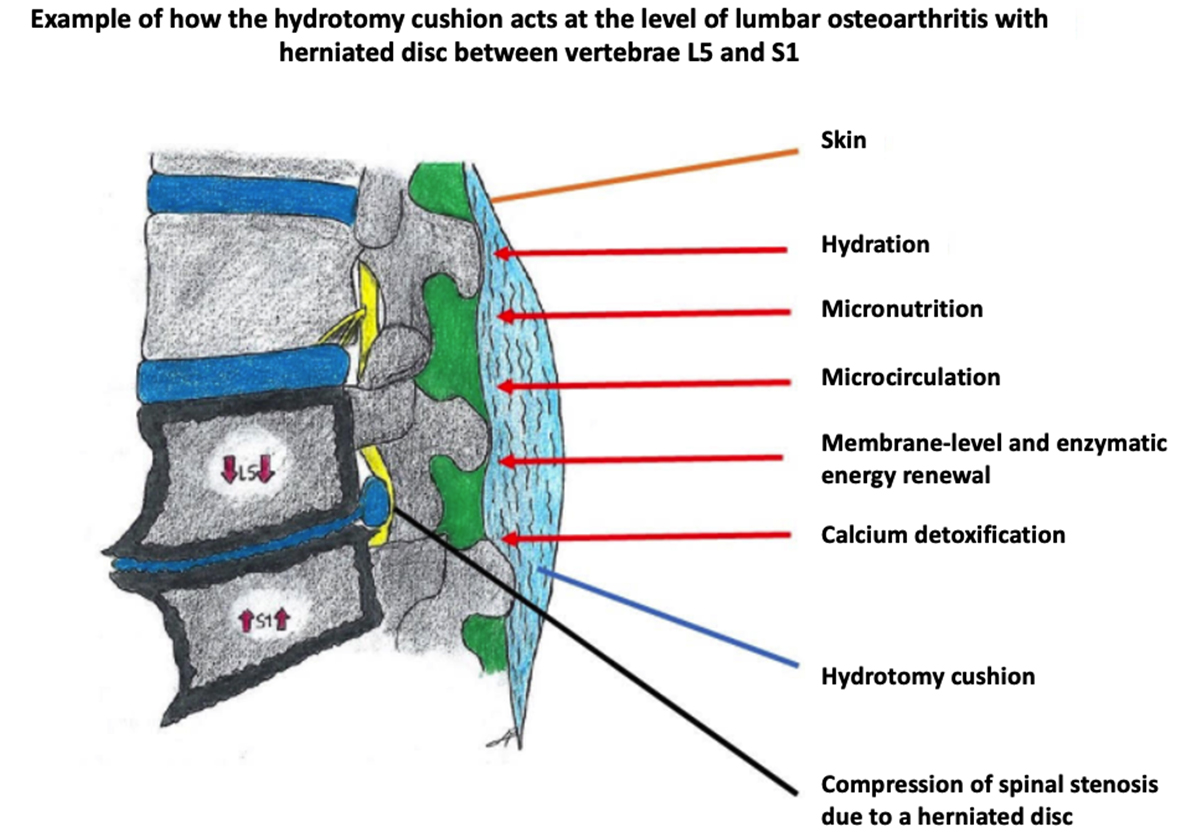
Percutaneous hydrotomy is a medical intervention which consists in intradermal or subcutaneous injection of a sterile saline solution (NaCl 0.9%) for the dilution of allopathic active compounds, in line with the market authorisation (MA). Hydrotomy can be used in combination with or prior to other therapeutic medicinal products in line with their scientifically established pharmacodynamic properties (Vidal). The “hydrotomy cushion” created by the sterile saline constitutes a therapeutic delivery vehicle for the other products, leading to localised regional diffusion helping to treat lesions in a targeted manner. The treatment can be administered discontinuously or continuously in private practice or outpatient services at the hospital using the “tumescent” technique.
MEDICAL TECHNIQUE: LOCOREGIONAL INJECTIONS FOR THERAPEUTIC PURPOSES
Percutaneous route for:
– Extracellular hydration
– Micronutrition (regenerative medicine)
– Therapeutic delivery vehicle.
Equivalent terms:
– Large dilutions
– Surface mesotherapy (subcutaneous infusion)
– Percutaneous hydrotomy
The SIHP is the only organisation authorised to provide training for practitioners in a medical context and declines all responsibility in case of illegal exercise of medicine.
Current status of the nomenclature
Locoregional injections for therapeutic purposes covers three techniques distinguished depending on the depth of injection.
These interventions are covered by the framework of the common classification of medical acts (CCAM) in France, and are therefore validated.
Administered at depth:
Intra-articular infusion of corticosteroids or hyaluronic acid, most often performed by rheumatologists or interventional radiologists.
- CODE: AHLB011
WORDING: Therapeutic infusion in the region of a spinal nerve at the rachidian cusp; unguided - CODE: AFLB007
WORDING: Epidural therapeutic injection of a pharmacological agent; unguided - CODE: MZLB001
WORDING: Therapeutic injection of a pharmacological agent into a joint or sinovial bursa of the upper limb; transcutaneous, unguided - CODE: NZLB001
WORDING: Therapeutic injection of a pharmacological agent into a joint or sinovial bursa of the lower limb; transcutaneous, unguided
In general practice, to ensure patient safety the pharmacological agent should not be injected directly into the joint at epidural level or into the sinovial bursa. Indeed, with unguided injections, these routes represent a risk of vascular or nerve breach, or injury to tendons or ligaments. The agent should preferably be instilled around the joint, at a distance from the joint to ensure safe use of the technique in general practice (e.g. when treating cervical vertebrae).
Percutaneous hydrology does not involve the injection of delayed action corticosteroids (risk of side effects and number of injections limited to 2 to 3 times per year) nor of hyaluronic acid into the joint, rather sterile saline (NaCl 0.9%) is injected orthogonally to the joint in line with its MA:
- Extracellular hydration
- Vehicle for therapeutic take-up
- Balance ion levels through chloride and sodium input
Administered at mid-depth:
Hypodermoclysis, or the continuous or discontinuous subcutaneous infusion of large quantities of sterile saline and drugs, performed by nurses in private practice, in hospital settings or nursing homes.
- CODE: AMI9
WORDING: Infusion treatment lasting up to one hour - CODE: AMI14
WORDING: Infusion treatment lasting more than one hour
Administered superficially:
Mesotherapy or intradermal injection of very low drug doses, most often performed by general practitioners.
- CODE: ANLB003
WORDING: Mesotherapy session for analgesia
Percutaneous hydrotomy is a “hybrid” local injection method for use in general medicine within the scope of the procedures listed above. It is listed in the common classification of medical procedures (CCAM) in France, and has been used for several decades.
The “hydrotomy cushion”, depending on its injection volume, constitutes a therapeutic supply vehicle between the deep and superficial planes regulated by the MA for sterile saline (NaCl 0.9%).
In fact, percutaneous hydrotomy differentiates these technical injection procedures based on the following two criteria:
- The depth of the injection, whether subcutaneous (12 mm) or intradermal (4 mm) and the region targeted: spine, shoulder, knees, fingers, etc.
- The injection volume, between 5 ml and 500 ml.
Applying the same criteria, the injection varies as follows:
- Single or multiple injections,
- Multipoint subcutaneous infusion can be applied for large areas (surface mesotherapy: spine)
In addition, during percutaneous hydrotomy low-dose peripheral local anesthaesia (xylocaine or procaine) is applied for analgesic purposes during infusion of 0.9% NaCl (tumescent technique used in cosmetic procedures): the hydrotomy cushion is thus targeted to the lesion. This technique has been used for several decades by all practitioners, particularly in general practice when placing stitches or extracting foreign bodies.
Hypodermoclysis (CODE: AMI 9 – AMI 14)
Subcutaneous administration of large quantities of physiological solutions. This technique is used to treat large infusion surfaces with drugs and NaCl 0.9% or glucose 5%.
It can be used to supply electrolytes, trace minerals, water-soluble and fat-soluble vitamins, among others.
Therapeutic indications: hydration and nutrition of geriatric and oncology patients, or as part of palliative care.
This technique is commonly used, and has been the subject of numerous scientific publications (see bibliographic references).
Mesotherapy (CODE: ANLB 003)
First developed by Dr Michel Pistor , mesotherapy consists of injecting small quantities of drugs “rarely and in the right place” to limit side effects.
Since 1997, Dr Pistor has encouraged the development of surface mesotherapy or percutaneous hydrotomy as the mesotherapy of the future, as a means to achieve “True cell washing” or “washout”.
Mesotherapy was recognized by the French Academy of Medicine in 1987, by ANAES (French health authority, now part of HAS) in 2001, and by the French National Order of Physicians in 2002. The technique is taught in medical faculties in Paris, Bordeaux, Lyon and Dijon.
Percutaneous hydrotomy uses allopathic conventional medical methods, optimizing their efficacy and safety (depth of injection, products used, large dilutions and small doses), and thanks to their local administration, very clearly reduces the adverse effects of drugs. Percutaneous hydrotomy thus corresponds to a very diluted mesotherapy technique developed over the past decades. It also makes it possible to treat the real causes of the disease at the pharmacological level (hydration, micronutrition, detoxification, regeneration, vaccination).
Percutaneous Hydrotomy relies on 3 medico-legal principles:
- The validity of local injection, which is a proven technique (listed in the CCAM).
- The use of local pharmacological agents for therapeutic purposes in line with their MA (Vidal).
- The freedom and independence of the doctor’s prescription within the scope of their professional practice and based on their expert knowledge of the patient’s medical history and therapeutic trajectory (article R.4127-8 of the French public health code).
- The patient’s free choice of practitioner (article R.4127-6 of the French public health code).
The International Society for Percutaneous Hydrotomy (SIHP) was set up to promote percutaneous hydrotomy techniques and the dissemination of knowledge in this field, to provide training in these techniques, to extend the scope of percutaneous hydrotomy research, and to facilitate communication between medical practitioners, healthcare workers and patients.
Take a look at the Origins and current concepts in Percutaneous Hydrotomy page

President of the SIHP:

Dr Bernard GUEZ
Nice, France
Advantages of the technique
The arthritic process is the result of biological and biochemical modifications at the osteoarticular level. The resulting mechanical inflammation corresponds to the secretion of chemical mediators, or cytokines, and pro-inflammatory substances (prostaglandins, interleukins, TNF alpha, and metalloproteases).
The mediators will modify the loco-regional homeostasis, causing physico-chemical variations (pH, joint osmolarity) in the joint with imbalances in intra- and extra-cellular or intra- and extra-vascular osmolarity, and water imbalances according to the semi-permeable membrane law (Donnan equilibrium). These effects will produce the clinical symptoms of inflammation (pain, redness, heat, swelling).
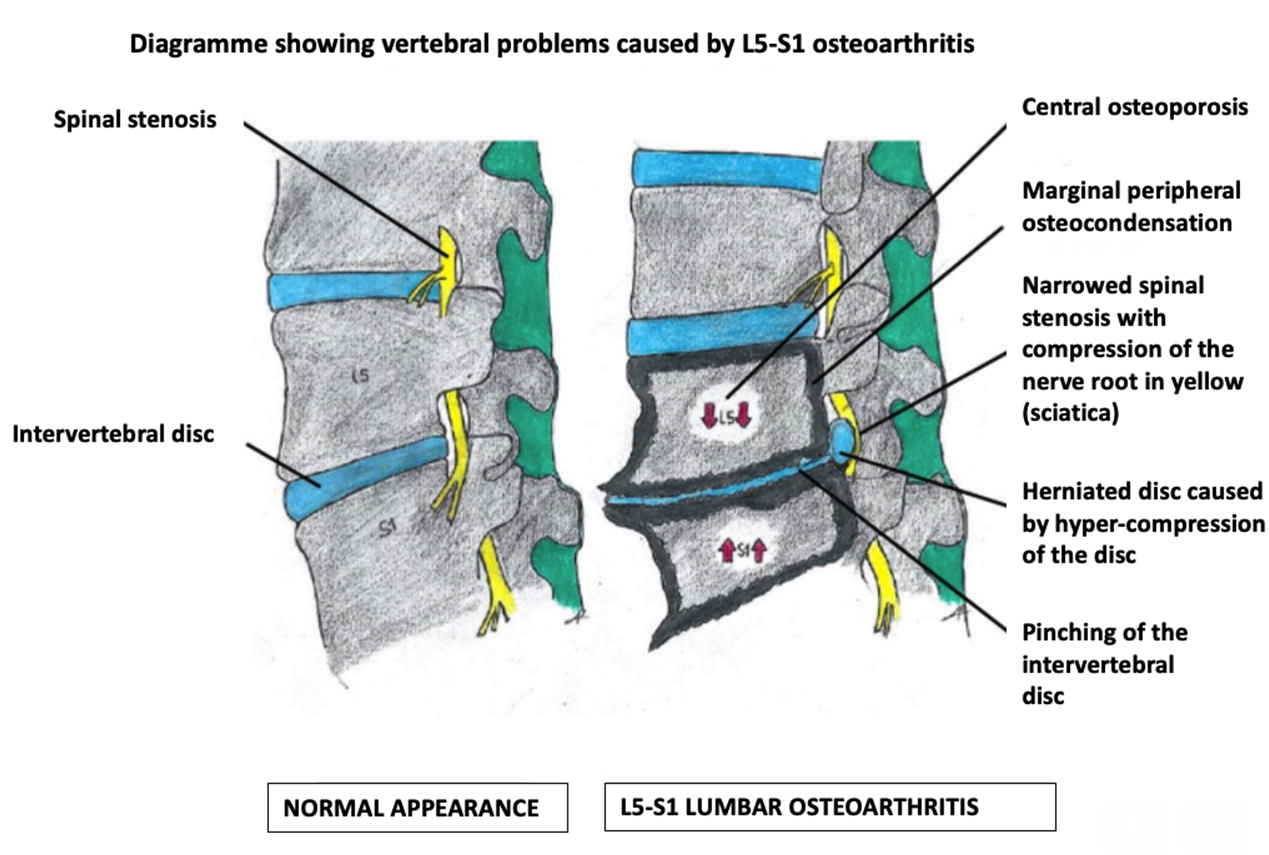
1) disc dehydration with pinched or slipped disc visible on MRI as a hyposignal
2) swelling of the surrounding vertebral plates with painful congestive phenomena (Modic signals).
Through the injection of large quantities of sterile saline solutions at physiological strength, percutaneous hydrotomy can re-establish the “iso-osmotic” equilibrium, thus regulating osmolarity and “inflammatory hypertonia”. In simpler terms, we could say that the effect of the extensive dilution is to “put out the fire”.
The opiod analgesics (grade 2) or morphine derivatives (grade 3) frequently used risk leading to habituation with pharmacological dependency in the mid-to-long term. Similarly, anti-epileptics reduce the pain threshold with several side effects. These drugs treat the symptom of pain without treating the hydromechanical cause regulating the plasticity of the osteoarticular ratios (bone, cartilage, discs, nerves, tendons, ligaments, synovial fluid, etc.).
After a conventional therapeutic trajectory, to their great satisfaction, many patients were able to discontinue their medication and saw their symptoms disappear thanks to percutaneous hydrotomy. They returned to normal functional activity, including sports activities.
Finally, the very low economic cost of this therapeutic alternative must be underlined as well as its undeniable ecological advantages.
Based on the body of evidence (studies, publications, communication to expert associations, bibliography, authorised opinions from healthcare professionals, expert analysis of medical records, several hundred testimonies from named patients, etc.), the health authorities should validate this technique, which has been in use for almost 40 years in private medical practice by hundreds of professionals, and is currently being tested with success in anti-pain centres.






radiological report
MRI of lumbar region
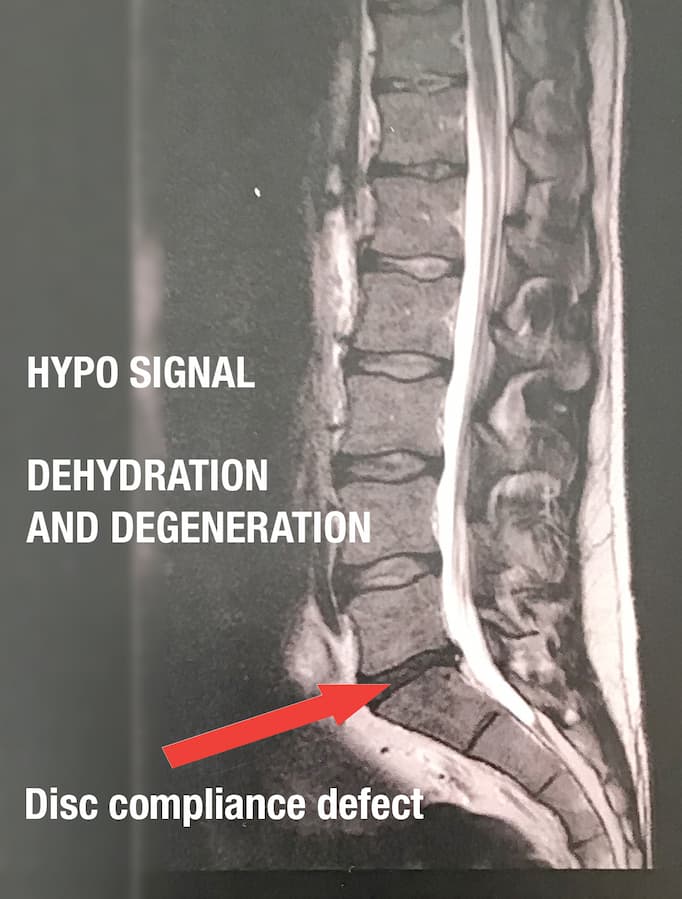
At the L5-S1 level: Some evidence of posterior somatic and inter-apophyseal bone degeneration. Degenerative dehydration and reduced height of the disc; presence of a bulging disc in left posterolateral position. A micro-tear of the annulus extending to the right paramedian and left internal foraminal level is visible, eliminating the left anterior epidural fat layer in contact with the S1 root pocket. This pocket remains at the pre-recessor level without obvious disco-radicular conflict. Absence of aqueductal or foraminal stenosis.
No sign of sacroiliitis.
Absence of mass at the para-latero-somatic level
Physical law of disc compliance.